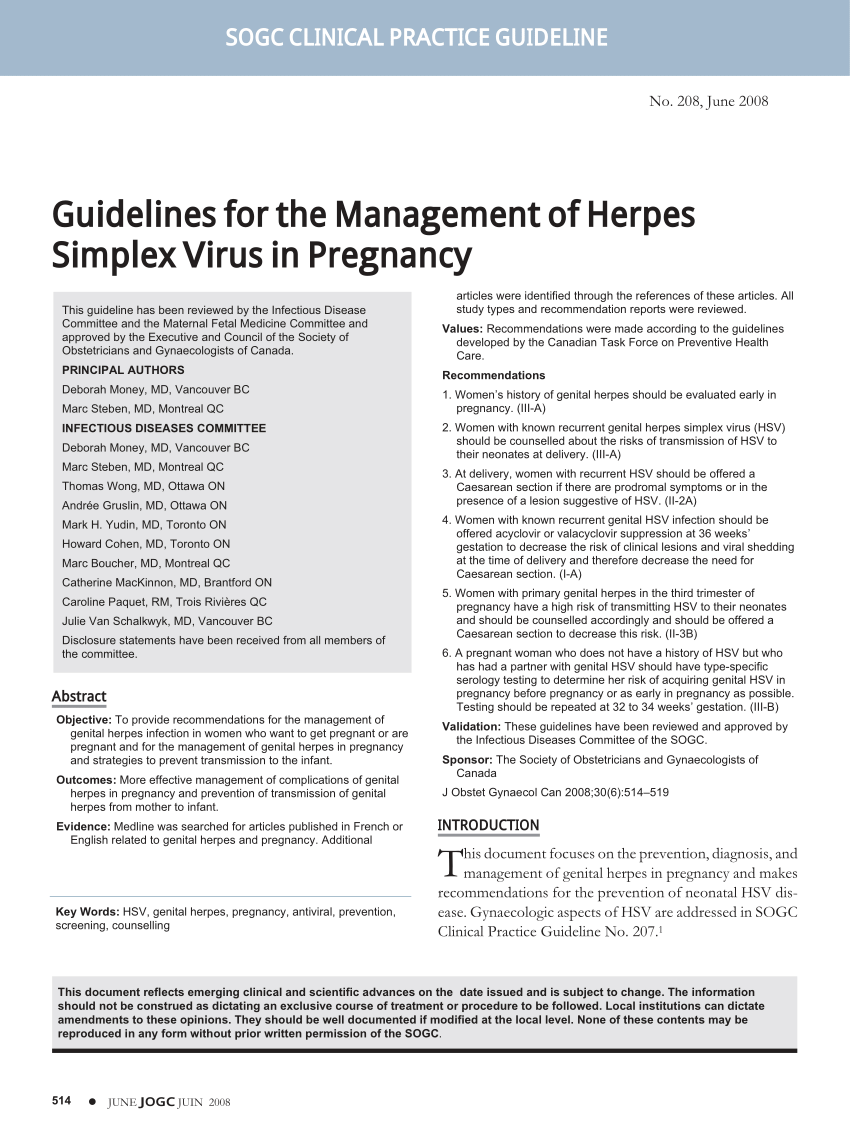
The major issues related to genital herpes infection in pregnancy will be reviewed here. Guidance is provided according to the type of maternal infection primary or recurrent and the gestational age at which infection occurred.
Recommended regimen for suppressive therapy of pregnant women with recurrent genital herpes Acyclovir 400 mg orally three times a day OR Valacyclovir 500 mg orally twice a day.
Hsv in pregnancy. Genital herpes simplex virus HSV infection during pregnancy poses a risk to the developing fetus and newborn. Genital herpes is common in the United States. Among 14- to 49-year-old females the prevalence of HSV-2 infection is 159.
ACOG has updated the guidelines for management of genital herpes in pregnancy. HSV transmission is via direct contact with an incubation period of 2 to 12 days. There are two types of HSV.
Most cases genital herpes are caused by HSV-2. A mother can infect their baby during delivery sometimes fatally. But if a woman had genital herpes before getting pregnant or if they are first infected early in pregnancy the chance that their.
Approximately 22 of pregnant women in the US. Two percent contract it during pregnancy thats 1 in 50 pregnant women. Two viral strains can cause genital herpes.
HSV-2 herpes simplex virus is the most common and typically spreads through sexual contact. Genital herpes simplex virus HSV infection during pregnancy poses a risk to the developing fetus and newborn. Genital herpes is common in the United States.
Among 14- to 49-year-old females the prevalence of HSV-2 infection is 159. Herpes is a very common sexually transmitted disease. In fact it is estimated that 20 to 25 of pregnant women are carriers of the herpes virus.
The vast majority of them will have children without experiencing any herpes-related complications for their babies. There is an increased incidence of viraemia in primary herpes infection in pregnancy. Herpes simplex infection should be considered in the differential diagnosis in the management of the acutely unwell pregnant woman.
Antiviral medications particularly aciclovir have been widely used in pregnancy without apparent adverse sequelae. Fortunately herpes is rarely transmitted to a baby during pregnancy since most newborns with HSV get it when they pass through an infected birth canal. If the amniotic sac breaks before birth very rarely the fluid in an infected birth canal can infect a.
Herpes simplex virus HSV infection is prevalent worldwide among women of childbearing age. During pregnancy the major concern of maternal HSV infection is transmission to the fetus as neonatal infection can result in serious morbidity and mortality. The major issues related to genital herpes infection in pregnancy will be reviewed here.
Recommended regimen for suppressive therapy of pregnant women with recurrent genital herpes Acyclovir 400 mg orally three times a day OR Valacyclovir 500 mg orally twice a day. Herpes simplex virus HSV infection is prevalent worldwide among women of childbearing age. During pregnancy the major concern of maternal HSV infection is transmission to the fetus as neonatal infection can result in serious morbidity and mortality.
The major issues related to genital herpes infection in pregnancy will be reviewed here. Neonatal herpes may be caused by herpes simplex virus type 1 HSV-1 or herpes simplex virus type 2 HSV-2 as either viral type can cause genital herpes in the mother. Approximately 50 of neonatal herpes is due to HSV-1 and 50 due to HSV-25 Most cases of neonatal herpes occur as a result of.
As the risk of herpes simplex virus HSV infection in pregnancy concerns the neonate rather than the mother the focus of this guideline is on managing maternal infection to reduce the risk of vertical transmission at birth. Guidance is provided according to the type of maternal infection primary or recurrent and the gestational age at which infection occurred. Herpes simplex virus HSV the most prevalent sexually transmitted infection is a DNA virus that has 2 major strains.
HSV-1 frequently is acq This common STI may be transmitted to newborns during delivery. However early recognition and treatment will improve outcomes. In response to these questions we summarize previous reports on herpes simplex virus 1 HSV-1 oral disease in pregnancy and briefly present 2 cases of primary gingivostomatitis in the first trimester of pregnancy resulting in a favourable outcome for both mother and infant.
In patients with HSV who are HIV-negative treatment reduces transmission of HSV to uninfected partners. During pregnancy antiviral prophylaxis with. Primary genital herpes infection in pregnancy is associated with an increased risk for perinatal transmission compared to recurrent HSV1 2.
HSV IgG antibody status can help to clarify whether the herpes episode is primary. Determining whether any HSV antibody present is of the same type as the HSV genital lesion assists with risk stratification. There is some evidence that HIV-positive women with genital HSV ulceration in pregnancy are more likely to transmit HIV infection independent of other factors.
If history of genital herpes offer daily suppressive aciclovir 400 mg TDS from 32 weeks to reduce the risk of transmission of HIV especially if vaginal delivery is planned.